What is MACRA?
Before MACRA, Medicare operated primarily on a fee-for-service (FFS) model, where providers were paid based on the volume of services rendered. This system often led to rising healthcare costs without necessarily improving patient outcomes. The Sustainable Growth Rate (SGR) formula, implemented in 1997, was intended to control spending by setting annual spending targets. However, SGR regularly threatened drastic cuts to physician payments, leading Congress to pass temporary "doc fixes" every year to avoid these reductions.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a bipartisan legislation signed into law on April 16, 2015, that significantly reformed how the federal government pays physicians. By transitioning Medicare away from a pure fee-for-service model, MACRA promotes value-based care, rewarding clinicians for the quality of services provided rather than the volume.
It repealed the sustainable growth rate formula and applies to eligible physicians and clinicians who provide services and treatment to Medicare patients. This is often referred to as the "pay-for-performance" model, as opposed to the previous "pay-for-service" model. The Quality Payment Program creates a new framework for rewarding clinicians who provide higher-value care.
"More than a Great" EHR "Customized For You"
What is Quality Payment Program (QPP)?
 The Quality Payment Program (QPP) is an incentive program created by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 and transforms the Medicare physician payment system from one focused on volume to one focused on value. It is designed to have the ability to reward high quality Medicare clinicians with reimbursement increases and at the same time reduce payments to clinicians who don’t meet the performance standards.
The Quality Payment Program (QPP) is an incentive program created by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015 and transforms the Medicare physician payment system from one focused on volume to one focused on value. It is designed to have the ability to reward high quality Medicare clinicians with reimbursement increases and at the same time reduce payments to clinicians who don’t meet the performance standards.
The Quality Payment Program or QPP permanently ended the complex, algorithm-based Medicare Sustainable Growth Rate (SGR) formula, which was considered by experts and practitioners as a flawed system.
If it had been implemented as intended, the SGR would have resulted in significant cuts in physician reimbursement. To avoid these, Congress had to pass a new law every year since 2003 to offset the decreases by authorizing the current fee schedule and a small increase for inflation.
Objectives of QPP
- To improve beneficiary population health
- To improve the care received by Medicare beneficiaries
- To lower costs to the Medicare program through improvement of care and health

- To advance the use of healthcare information between allied providers and patients
- To educate, engage and empower patients as members of their care team
- To maximize QPP participation with a flexible and transparent design, and easy to use program tools
- To maximize QPP participation through education, outreach and support tailored to the needs of practices, especially those that are small, rural and in underserved areas
- To expand Alternative Payment Model participation
- To provide accurate, timely, and actionable performance data to clinicians, patients and other stakeholders
- To continuously improve QPP, based on participant feedback and collaboration
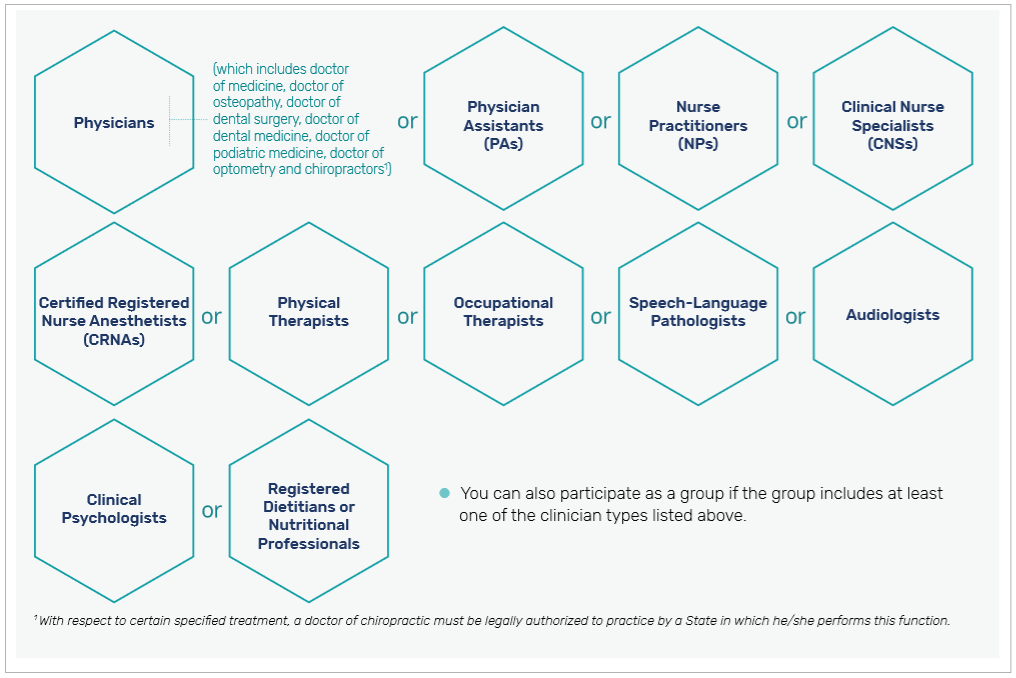
Who can Participate in QPP?
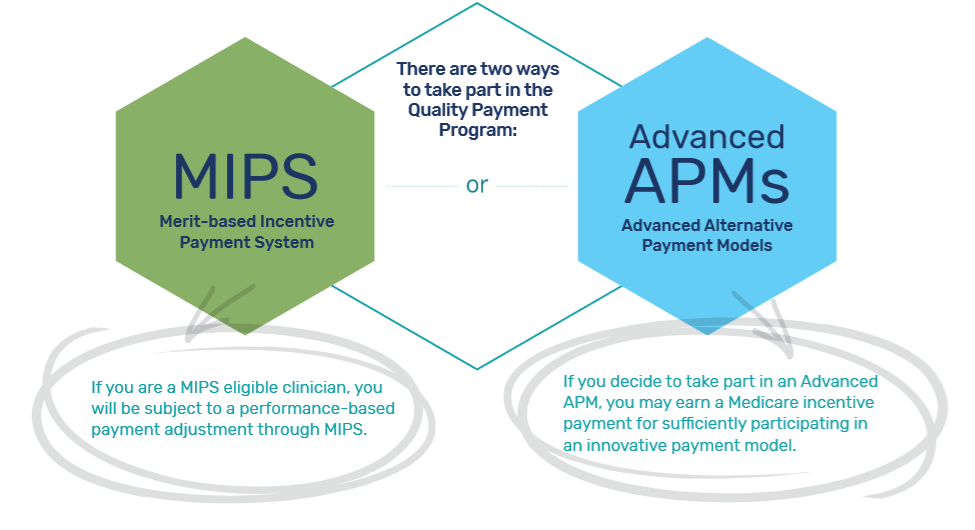
QPP Tracks
QPP defines two tracks for healthcare providers to participate and be reimbursed for quality-based care:
- Merit-based Incentive Payment System (MIPS)
- Alternative Payment Models (APMs).
Impact of MACRA on Physicians
- Future Medicare payments will be dependent on participation and performance in these programs. Because CMS will base its payment adjustments for both MIPS and APMs on performance from two calendar years prior, practices need to take this into consideration for their revenue cycle strategies and income outlook.
- To streamline reporting and accessing of data, practices may need to invest in technology tools such as certified EHRs that offer interoperability/sharing of data across systems.
- Physicians will need education and training for themselves and their staff, to understand the details of the new law and how it affects them. While this can this be the first and main obstacle to participating, investing the time and resources to make sure this is in place can have significant pay-offs down the road.
- Smaller practices who want to participate in virtual groups or APMs will need to collaborate and improve partnerships locally and regionally.
What Should Small Practices do to Get Ready for MACRA?
1. Understand the changes
Clinicians will need to wrap their heads around how the performance categories are scored, how measures are reported, as well as what the reporting timelines are. Detailed information and tools regarding these topics are available at https://qpp.cms.gov/.
2. Analyze the financial impact to your practice
According to a recent article in Health Affairs, adjustment ranges for Medicare payments under MIPS can actually be larger than the publicized amounts. Health Affairs notes that "For example, in 2017, adjustments could have ranged from -4% up to +22% (comprised of the generally publicized amount of 4%, scaled by a factor of 3 and inclusive of a 10% exceptional performer bonus)."
It is important to keep in mind that while positive adjustments are always welcome, negative adjustments are also a reality and can have a significant impact on the practice's revenue and bottom line.
3. Embrace change
The use of certified EHR which meets 2015 Health IT Certification Criteria is a key requirement in the MIPS Promoting Interoperability Category. Additionally, using a certified EHR supports the other performance categories by providing a tool that helps enhance patient safety and clinician communication, among others. Here are 6 Questions You Must Ask Your HER Vendor to Optimize Your EHR for MACRA
4. Identify and use available resources
- Find and use the large amount of free informational tools provided by CMS online, as well as other FAQs and tip sheets by other authoritative organizations. Some links are provided at the end of this article, for reference.
- Contact on-the-ground resource organizations established by CMS.
- Evaluate whether using a third-party intermediary to collect and submit data on your behalf may be helpful.
- Discuss their goals and requirements with their EHR and Health IT- related vendors.
- Assess whether joining an APM is beneficial and viable.
MACRA and the QPP represent a sweeping revamp of Medicare payments to emphasize value-based care, and it affects providers and practices at every level. Its impacts extend from how care is provided, to how it is reported, evaluated, and rewarded. It affects clinical practice, patient outcomes, and practices' financial growth.
While not perfect, it has been evolving, due in part to the feedback from the healthcare community. Physicians and practices who pay attention, adapt, and provide feedback that may help influence future iterations of this program are helping both their patients and themselves to grow and thrive in this new reality.
Frequently Asked Questions
How does MACRA affect small and independent practices?
MACRA includes provisions like the "small practice bonus" and simplified reporting to support small and independent practices, ensuring they can participate effectively in MIPS without facing excessive administrative burdens.
What role does technology play in MACRA compliance?
Technology, such as certified EHR systems, helps providers track performance metrics, submit MIPS data, and ensure quality reporting, making it essential for successful MACRA participation and avoiding penalties.
What is the difference between MIPS and APMs under MACRA?
MIPS adjusts payments based on performance across four categories, while APMs offer higher incentives for adopting innovative, coordinated care models with lower financial risk.
What happens if a clinician does not participate in MACRA?
Non-participation results in automatic negative payment adjustments under MIPS, which can significantly impact Medicare reimbursements over time.
How does MACRA align with value-based care goals?
MACRA prioritizes quality outcomes, cost efficiency, and patient satisfaction, aligning Medicare reimbursements with the broader goal of transitioning to value-based care systems.
Resources:
CMS QPP Website: https://qpp.cms.gov/
CMS Small Practice Fact Sheet: https://qpp.cms.gov/about/resource-library
AAFP FAQs https://www.aafp.org/practice-management/payment/medicare-payment/macra-101/faq.html
ACR Resources: https://www.acr.org/Practice-Management-Quality-Informatics/MACRA-Resources



