Save time and reduce administrative burden with practice management software including tools for scheduling, billing, insurance verification, reporting, and more. From scheduling and billing to insurance verification and reporting, our platform automates routine tasks, allowing your staff to focus on patient care.
Discover how our integrated cloud-based software can revolutionize your operations, reduce administrative overhead, and improve patient outcomes.
👉 Request a Free Demo Now and join thousands of healthcare providers leveraging smarter workflows and innovative technology for better care delivery.





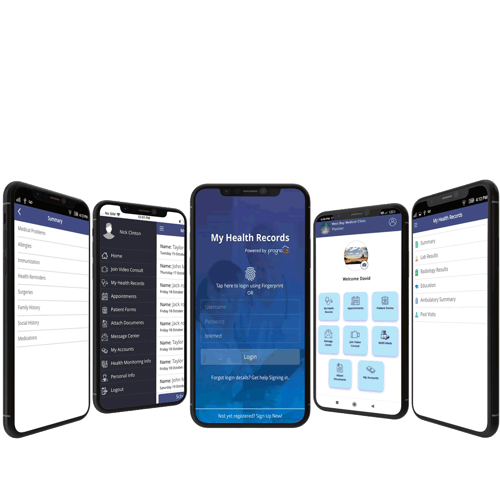
Universal Secure Access: Connect seamlessly via any internet-enabled device—tablets, smartphones, PCs, or Macs—with two-factor authentication ensuring data security. Send appointment reminders, view lab results, and streamline communication.
Integrated Patient Tools: Check and request appointments, view statements, and ask for prescription refills. Facilitate rapid communication with other healthcare providers, ensuring cohesive patient care without delays.
Boosted Engagement & Efficiency: Enhance patient engagement, loyalty, and health outcomes. Simplify administrative tasks with online forms and patient-driven scheduling, all within a HIPAA-compliant environment.

Streamlined Team Communication: Advanced internal messaging systems ensure seamless synchronization among staff members. With these tools, communication gaps are eliminated, fostering unified care and bolstering administrative efficiency.
Direct & Secure Patient Interactions: Prioritizing the bond between patients and healthcare providers, integrated tools facilitate appointment reminders, health updates, and real-time feedback. This fosters trust, ensuring patients remain informed and engaged every step of their health journey.
Integrated Alerts & Automated Notifications: Tailored notifications and alerts enhance patient adherence, ensuring they’re kept abreast of upcoming appointments, medication schedules, and essential health milestones.
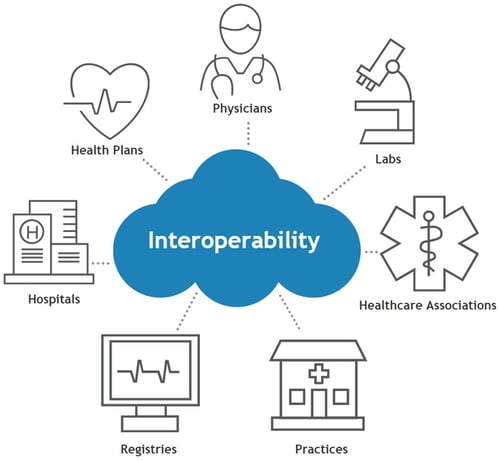
Advanced System Synchronization: RevenueXL stands out in its ability to harmoniously interact with a multitude of platforms, breaking data silos and ensuring a comprehensive patient care approach by maintaining up-to-date information across various systems.
Open System Adaptability: Embracing an Open API infrastructure, RevenueXL offers unparalleled flexibility, allowing for easy integration with a wide range of third-party apps and tools, positioning practices to remain adaptable to the ever-evolving healthcare tech landscape.
Unified Healthcare Data Framework: Our commitment to real-time data synchronization ensures every stakeholder has access to the most current and comprehensive patient data, fostering effective clinical decisions and enhanced patient outcomes.

Holistic Patient Care: Bridging geographical barriers, the software offers patients, especially in underserved regions, swift access to expert diagnoses, treatments, and real-time care.
Optimized Virtual Engagement: Our custom mobile app blends text, email, and video, simplifying remote consultations and bolstering patient-provider interactions while lowering costs.
Unparalleled Access & Integration: Within a HIPAA-compliant framework, physicians can access patient charts, prescribe medications, and seamlessly liaise with other healthcare departments.
Scalability and Connectivity: Perfect for solo practitioners to large medical facilities, RevenueXL ensures smooth communication with essential healthcare entities, centralizing critical interactions.

Practice management is the coordination and administration of the financial, operational, and administrative tasks that enable a medical practice to run smoothly and efficiently. It encompasses key areas such as financial management, patient care coordination, human resources, compliance, technology integration, and operational oversight.
At its core, practice management ensures that healthcare providers can focus on delivering quality patient care while minimizing administrative burdens. This is achieved through systems and strategies that streamline appointment scheduling, billing, coding, revenue cycle management, and compliance with regulations like HIPAA and MACRA. The adoption of practice management software is central to achieving these objectives, offering solutions for automated workflows, secure patient data handling, and seamless integration with EHR systems.
The role of a practice manager is pivotal, as they oversee tasks such as financial planning, quality assurance, staff training, and patient engagement initiatives. By implementing technologies like patient portals, telehealth, and automated reminders, practice management fosters a patient-centric environment that enhances satisfaction and outcomes.
In an evolving healthcare landscape shaped by regulatory changes and technological advancements, practice management ensures operational efficiency, financial sustainability, and improved care delivery, making it indispensable for modern medical practices.
Customized templates and workflow for your specialty to accelerate adoption, encounter documentation speed and patient care.
Ready to see how RevenueXL can help your medical practice improve efficiency and enhance quality of patient care?
Fill out the form below to schedule your customized demo.
Customizable workflow,templates, and content created for your specialty
Two service options to ensure your MU attestations are smooth and hassle-free
Easily share lab results, appointment reminders, statements, and prescriptions with patients
Patients can complete secure credit card transactions from the comfort of their homes
RCM services process statements and handle claims while you connect with patients
Designed for specialty, from Allergy to Urology
Quickly prescribe or refill prescriptions and send straight to the patient’s preferred pharmacy
Surescripts feature allows you to monitor patient prescription usage and medication adherence
Friendly, knowledgeable 24/7 support staff available via support ticket, phone, email, or chat
Quickly enroll your practice with 3rd-party payers and begin seeing patients
Electronically sign documents within EMR or patient portal with HIPAA-compliant e-signature feature
HL-7 interfacing and CCHIT & ONC-ATCB-certified, conforming to critical security and functionality measures
Communicate with practice & labs, radiology, pharmacies, & referring doctors
Convenient with iPhone & iPad
© 2021 RevenueXL Inc. All rights reserved. Unauthorized Reproduction Prohibited - Legal Notice.