Introduction
In the evolving healthcare landscape, digital solutions like Electronic Health Records (EHR) and Electronic Medical Records (EMR) have revolutionized how patient data is managed and shared. While the two terms are often used interchangeably, they serve distinct purposes.
The difference between EHR vs. EMR isn’t just technical—it impacts patient care, practice efficiency, regulatory compliance, and interoperability across healthcare networks. For healthcare providers, understanding these distinctions is crucial for making informed decisions when investing in health IT systems.
The difference between EHR and EMR significantly impacts patient care, practice efficiency, regulatory compliance, and the seamless exchange of healthcare information. While an EMR emphasizes the medical aspects of patient care within a single provider’s records, detailing their medical history, treatments, and diagnoses specific to that practice, an EHR is designed for interoperability and ensure coordinated care. It provides a comprehensive view of a patient’s overall health, integrating medical, lifestyle, and wellness data and allows seamless sharing across multiple providers and organizations, fostering more coordinated, informed, and patient-centric care.
Let us learn more about the differences below.
| Nature of Difference |
Electronic Medical Records (EMR) | Electronic Health Records (EHR) |
|---|---|---|
| Scope of Information | Contains the patient’s medical history, diagnoses, medications, and treatment plans, typically within a single organization. | Designed for access and sharing across providers, networks, and geographies, offering a complete, longitudinal health record. |
| Interoperability | Limited or no sharing capabilities with other systems, hindering collaboration outside a single organization. | High interoperability enables secure sharing of data among authorized healthcare providers across different settings. |
| Care Coordination | Limited tools for care coordination, often restricted to internal communication within the organization. | Specifically designed to facilitate care coordination across multiple providers and settings, enhancing collaboration. |
| Analytics & Population Health Management | May include basic or no tools for analytics and population health management. | Offers advanced analytics for identifying trends, improving outcomes, and managing population health effectively. |
This structured comparison highlights how EHRs extend beyond the capabilities of EMRs, making them more suitable for integrated and collaborative care environments.
Real-World Use Cases for EHR and EMR
EMR in a Private Practice
A family physician operating a small clinic might rely on an EMR to track patient visits, diagnoses, and lab results over time. The focus remains on internal data management without extensive interoperability requirements.
Example Scenario:
A patient visits the same doctor annually for check-ups. Their health history, medications, and lab results are securely stored in the EMR, helping the physician make informed decisions.
EHR in a Multi-Specialty Hospital
In contrast, a multi-specialty hospital using an EHR benefits from seamless data sharing across departments. If a patient visits the cardiology department and later sees an endocrinologist, the EHR ensures that both specialists have access to the same data.
Example Scenario:
A diabetic patient with heart complications can receive synchronized care from both cardiologists and endocrinologists without redundant tests or conflicting treatments.
Advantages of EHR Over EMR
Enhanced Interoperability
EHRs allow different healthcare providers, specialists, and even hospitals to share patient records seamlessly. This ensures coordinated care and minimizes redundancies.
Patient Engagement and Empowerment
EHRs offer patient portals where individuals can view test results, schedule appointments, and communicate with healthcare providers. This leads to greater engagement and improved health outcomes.
Regulatory Compliance
EHRs are designed to meet national healthcare regulations like HIPAA and Meaningful Use standards, ensuring legal compliance while protecting patient privacy.
Enhanced Clinical Decision Support
EHRs often include decision-support tools, reminders, and alerts to help providers make evidence-based decisions quickly.
Data Analytics and Reporting
With robust reporting tools, EHRs help healthcare providers analyze data trends, identify potential risks, and optimize workflows.
When to Choose EHR vs. EMR?
Practice Size:
- Small, Independent Practices: EMR might suffice.
- Larger Multi-Specialty Practices or Networks: EHR is more suitable.
Interoperability Needs:
Practices requiring collaboration across facilities need EHRs.
Patient Engagement Goals:
If enabling patient portals and communication tools is a priority, opt for EHR.
Budget Constraints:
EMRs are often more cost-effective for smaller practices.
Compliance Requirements:
Practices needing enhanced reporting and regulatory compliance should prefer EHRs.
Recommendation:
Evaluate your long-term goals, technical requirements, and growth plans before making a decision.
The Future of EHR and EMR
AI and Predictive Analytics:
EHRs are integrating AI tools to predict disease patterns, flag early warning signs, and enhance decision-making.
Telehealth Integration:
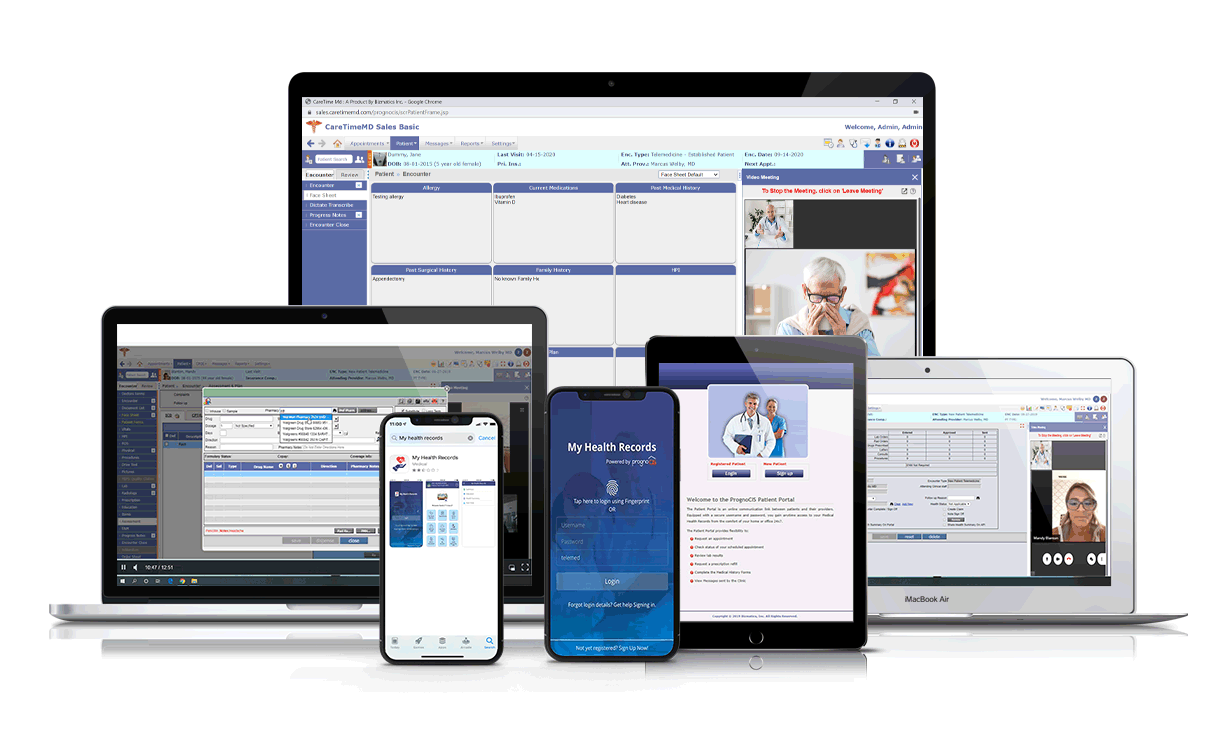
Both EMR and EHR platforms are evolving to seamlessly integrate with telemedicine solutions, supporting virtual consultations.
Data Security and Privacy:
Future systems will focus heavily on encryption and data protection protocols to meet global security standards.
Mobile Accessibility:
Accessing records via mobile devices is becoming standard, improving efficiency for providers and patients.
Conclusion
The debate between EHR vs. EMR isn’t about which is superior—it’s about which is better suited to your practice’s needs. Choosing the right system is an investment in better care, operational efficiency, and long-term success.
Explore how RevenueXL’s tailored solutions can help your healthcare practice thrive.
👉 Learn More About Our EHR Solutions






